Wil our N.H.S. EVER BE LIKE THIS
- 25 April 2022 02:58376537Part of our family live in Tampa in the USA very nice part to live in,anyway they had to go for appointment at their local Hospital, they were given the time for that,when they drove there a nurse was waiting,with her was a chauffeur who asked for their car keys then he took it away,there was no Waiting the nurse escorted our family members to where the Dr was waiting for them after their concentration with the Dr they were escorted back to the front of the hospital where their car was waiting it had been washed and polished and valeted inside to a very high standard they were given back the keys and off they went,all at no ex cost,will we see our N.H.S. going that way.



- 25 April 2022 08:58376545I’m sure In the USA they have to pay for health provision.In this country it is free however we still pay through taxes .My income on my small pension was highly taxed and those who do work pay high nation insurance.
. - 25 April 2022 13:27376547Health insurance premiums in the USA are very costly which is why many people do not have access to the care they need. I’m not sure I care if my car is cared for - nothing is free and it will all be part of the package they have signed up to.
- 1 August 2022 15:52378064"We are living in very strange times, and they are likely to get a lot stranger before we bottom out"
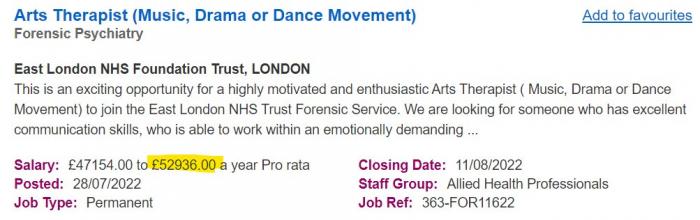
Dr. Hunter S Thompson - 8 August 2022 14:48378143More non jobs!"We are living in very strange times, and they are likely to get a lot stranger before we bottom out"
Dr. Hunter S Thompson - 8 August 2022 15:28378144"We are living in very strange times, and they are likely to get a lot stranger before we bottom out"
Dr. Hunter S Thompson - 9 August 2022 10:39378152"We are living in very strange times, and they are likely to get a lot stranger before we bottom out"
Dr. Hunter S Thompson - 9 August 2022 16:21378155I think the good Captain with all these job adverts is either bored stiff or has too much time on his hands.

We all know the NHS wastes money.-----------------------------------------------------------------------
I try to be neutral and polite but it is hard and getting even more difficult at times.
------------------------------------------------------------------- - 9 August 2022 18:45378159Jan Higgins wrote:I think the good Captain with all these job adverts is either bored stiff or has too much time on his hands.

Yup. Back to chugging up ditches tomorrow.
I may be some time ............Jan Higgins likes this"We are living in very strange times, and they are likely to get a lot stranger before we bottom out"
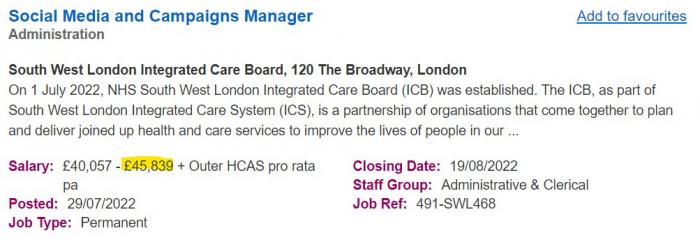
Dr. Hunter S Thompson - 15 October 2022 17:35378826"We are living in very strange times, and they are likely to get a lot stranger before we bottom out"
Dr. Hunter S Thompson - 16 October 2022 08:39378841"...ambitious EDI strategy which sets out our vision which is to be 'consciously inclusive in everything we do for our patients, communities and colleagues'".
Lord give me patience but hurry. Now look NHS, it's easy - the human body is a machine; it can go wrong in a myriad of different ways; your job is to fix it when it does and to service it before it does. If you feel you can't manage that, don't become a medic. Start by being a Kwik Fit fitter and see how you get on with cars.(Not my real name.) - 16 October 2022 09:44378843The NHS management side from the bottom rung to the top seem to be quite simply not up to the job and have not for a very long time.
I feel sorry for all the front line medics who try and make the best of the appalling situation we now seem to be in because there are simply not enough of them. I would be willing to bet that the office manager numbers are still more or less the same even though my practice has closed their Health Centre patient side.
A personal example I am supposed to have blood tests every 6 months because of medication I take, because of the covid pressures I was not expecting the same time frame. But I had my first since the end of 2018 was a week ago, when I will find out the result is anyone's guess, luckily I have had no problems in the past so fingers crossed all ok.-----------------------------------------------------------------------
I try to be neutral and polite but it is hard and getting even more difficult at times.
------------------------------------------------------------------- - 19 October 2022 13:18378884Keeping it local:-
The Governor of East Kent Hospitals Trust today resigned ahead of the publication of a 'harrowing' report into a decade of maternity failings.
Alex Lister claimed there was a 'cancer at the top of the organisation', accusing trust bosses of continuing to 'mislead, obfuscate, bully and conceal vital information'.
He said the trust's communications were 'rotten to the core'.
In a brutal resignation letter leaked this morning, he said: 'For the sake of our NHS heroes, the bereaved families, the children who will never grow up, and the public who rely on us, you must clean house.
'Replace the spin doctors with real doctors and be brave enough to say publicly what we all believe to be true.'
Mr Lister added: 'I believe officials on six-figure salaries continue to mislead, obfuscate, bully and conceal vital information.'
https://www.dailymail.co.uk/health/article-11331601/Lead-governor-East-Kent-Hospitals-Trust-resigned-just-HOURS-release-harrowing-report.htmlJan Higgins likes this"We are living in very strange times, and they are likely to get a lot stranger before we bottom out"
Dr. Hunter S Thompson - 19 October 2022 13:26378885I am just listening to the report, there can be absolutely no excuse for the appalling care and loss of life.
https://www.bbc.co.uk/news/uk-63298087-----------------------------------------------------------------------
I try to be neutral and polite but it is hard and getting even more difficult at times.
------------------------------------------------------------------- - 14 November 2022 15:44379224I've been trying to get an appointment to see my doctor for ages.
I finally saw him today and showed him the rash on my scrotum.
He just ignored me and walked straight past me pushing his shopping trolley."We are living in very strange times, and they are likely to get a lot stranger before we bottom out"
Dr. Hunter S Thompson - 18 November 2022 12:17379266Fun Fact
The NHS spent £65 million on translation services £56 on foreign language interpretation and £9 on sign language in 2019/20.
In Spain if you go to hospital and cannot speak the language you have to bring your own interpreter."We are living in very strange times, and they are likely to get a lot stranger before we bottom out"
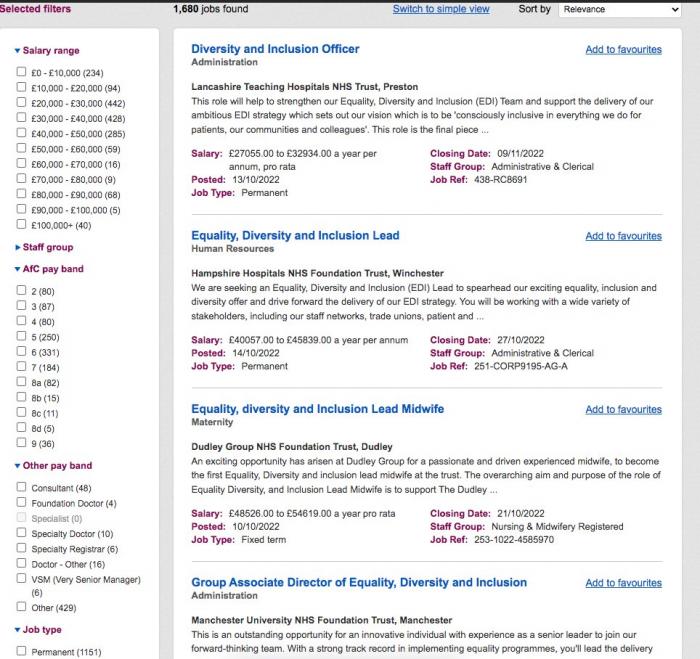
Dr. Hunter S Thompson - 8 December 2022 11:46379494Envy of the world?
“How did you go bankrupt?" Two ways. Gradually, then suddenly.” ― Ernest Hemingway,
"We are living in very strange times, and they are likely to get a lot stranger before we bottom out"
Dr. Hunter S Thompson - 17 December 2022 21:12379595"We are living in very strange times, and they are likely to get a lot stranger before we bottom out"
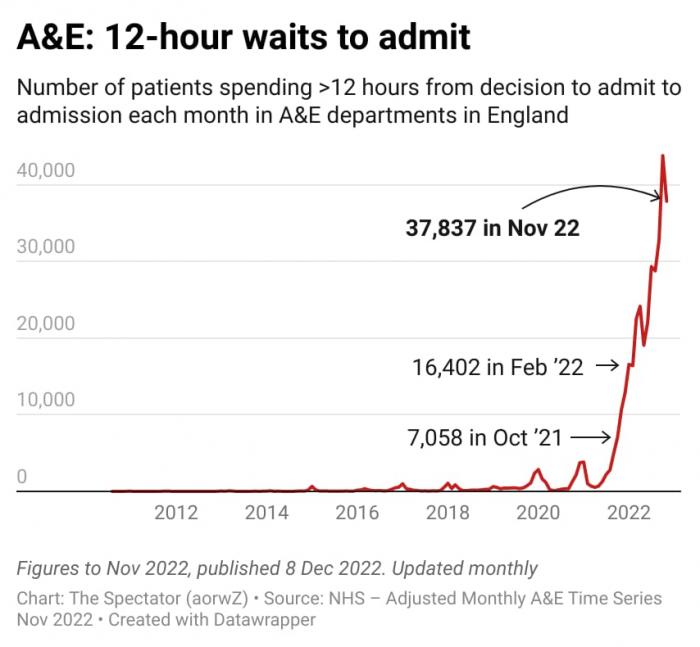
Dr. Hunter S Thompson - 17 December 2022 21:32379596Daily Telegraph today
HEALTH SERVICE
Share
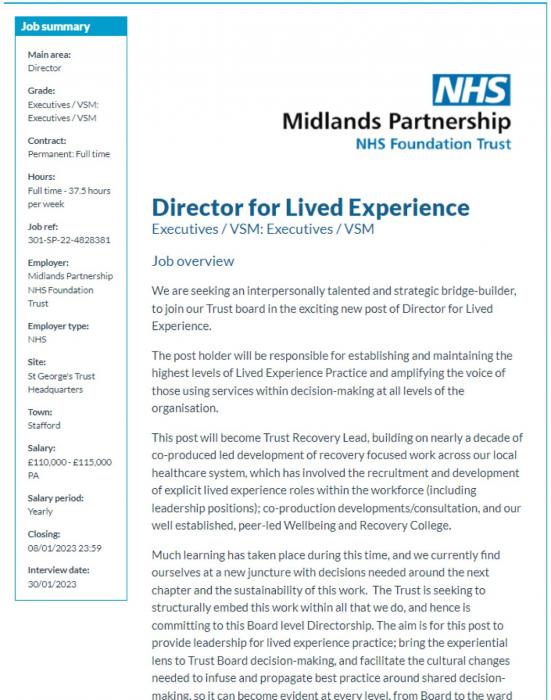
NHS hires £115,000 ‘lived experience’ tsars
EWAN SOMERVILLE
THE NHS has hired an army of “lived experience” tsars on salaries of us to up £115,000, despite ministers vowing to fight a war on waste.
Midlands Partnership NHS Foundation Trust (MPFT) is recruiting a “director for lived experience” who must have “experience of a life-altering health condition” and “significant power imbalances” in their use of health services. The tsar will “ensure brave spaces” for people to give feedback and be based at St George’s Hospital, in Stafford, on a salary of £110-115,000 per year – four times that of a newly-qualified nurse or junior doctor.
They should also “seek out and heavily involve ‘seldom heard’, under-represented and/or disadvantaged groups” and be a “strategic bridge-builder”, a job advert says.
An NHS source said such power imbalances would include “feeling disempowered, vulnerable and that an individual’s own voice is lost” in using mental or physical health services.
The trust claims it is the first such board-level position in the health service, but The Daily Telegraph has identified at least 20 “lived experience” job titles across seven NHS trusts, being paid a total of at least£600,000.
Last night, the NHS was accused of “inventing problems and creating jobs to solve them”, as a former health minister called for cash to go into direct patient care.
An NHS spokesman said: “[While] the roles [are] not funded nationally, NHS England is working to reduce the number of its own job posts by 30-40 per cent with taxpayers’ money redistributed to fund patient care.” - 18 December 2022 00:12379597FT Tpday
Two and half years ago, as an unknown virus swept the nation, I found hope in an unlikely place: the NHS. Hospital doctors and nurses were gripped by a spirit of camaraderie and can-do, in stark contrast to the weary burnout we see today. As the NHS approaches its high noon, with the cataclysmic combination of nurses on strike for the first time in a century and ambulance workers to walk out next week, I remember that glimpse of a way to do things better.
I had a strange and privileged experience in 2020, as a temporary adviser to the Department of Health. Sitting in the dysfunctional centre of government, which had a vacuum where a prime minister should have been, I briefly witnessed a fragmented system come together to do what frontline staff thought was right for patients, liberated from some of the usual protocols.
When Covid hit, dental hygienists, surgeons and physiotherapists retrained as ICU nurses. Care workers gave insulin injections and wrote death certificates. Even the BMA, that bastion of conservatism, had to drop its attempt to stop medical students looking after Covid patients. At one Zoom conference I attended, organised by a surgeon, hundreds of GPs and consultants said passionately that they no longer wanted to work in silos; that they were collaborating in new ways; that they had been liberated from HR jargon and form-filling.
“We must never go back” was their refrain in the spring of 2020. But we have. In less than a year, the bureaucracy reasserted itself. Retired doctors who volunteered to help with the vaccine rollout were required to undertake 18 training modules, including one on preventing terrorism.
Mind-numbing “guidance” gushes from the centre as strongly as ever. Nurses tell me of money being spent on “comms” teams rather than healthcare. Surgeons tell me they are doing fewer operations than pre-pandemic because of infection control measures, failing computer systems and theatre staff turning up late. Last year, 12,600 operations were cancelled because of administrative errors. When professionals are exhausted, facing a backlog of 7mn patients, and pay is falling in real terms, it is hardly surprising that so many are leaving, or on strike.
Where has all the extra money gone? A new report from the Institute for Fiscal Studies finds that the NHS is treating substantially fewer patients than it was before the pandemic, despite having more staff and more money (its current budget is £180bn). The usual explanation for poor performance is that demand is outpacing funding. But the IFS suggests that the money is being spent on the wrong things.
The past three years have seen large increases in the employment of consultants, junior doctors, nurses and clinical support staff. There were 10 per cent more consultants, nurses and health visitors in July 2022 than in July 2019. This doesn’t seem to be translating into higher productivity, partly because some patients are sicker and require more treatment, and partly because beds are being “blocked” by elderly people who are fit to discharge but unable to access social care.
Yet the analysis also suggests that many of the new hires are at senior or junior ranks, not in the middle. We risk losing the backbone of the NHS: the registered nurses who manage the day-to-day delivery of care. There are more specialists and fewer generalist GPs and community nurses who can help patients at an earlier stage.
Even with all these extra staff, there are still so many vacancies. Why? One NHS insider explained to me that when funding rises, so does the number of funded posts. So boosting resources automatically creates a workforce shortage. I have been shown that the number of “establishment” posts (required staffing levels) jumped up when new funding was announced. This is insane.
For decades, debate about staff numbers has been the currency of politics. Successive governments have paraded “more nurses, more doctors” as a cure-all for warding off criticism. But when the NHS has 200,000 more staff than it did in 2012, and 1.2mn staff overall, it is time to ask about how staff are being used, not just how many they are. “Staff undoubtedly feel stretched” write the IFS authors. “But it is not obvious that adding more staff or money would immediately unclog the system”.
There is an opportunity here to change the conversation. Wes Streeting, the Labour shadow health secretary, seems refreshingly ready to do just that. “I’m not afraid to take on vested interests,” he said recently — including in his own party.
If the NHS and its frontline are to do their best for patients, we need a revolution in organisational management. General Sir Gordon Messenger, former deputy chief of the defence staff, recently reviewed the state of NHS leadership and concluded that there has been “institutional inadequacy” in the way managers are “trained, developed and valued”. Even if overhaul is tiring, change is now vital, to restore autonomy, respect and proper support.
Covid posed an immediate threat which spurred NHS professionals to rise to the challenge of their vocation. This crisis feels very different: a desperate grind to get through each day, where everything is urgent.
Nigel Edwards, CEO of the Nuffield Trust, used to joke that in the NHS: “next week is strategic; the week after is the unimaginable future”. It’s no longer a joke. Unless leaders can show there is a better future, no amount of new staff will fix the problem.
camilla.cavendish@ft.com"We are living in very strange times, and they are likely to get a lot stranger before we bottom out"
Dr. Hunter S Thompson